
Tests verify if uncertified N95 masks are effective

Still today, states are scrambling to find N95 respirator masks, the kind that seal against the face and filter out infectious particles, protecting frontline workers from inhaling the coronavirus. A national shortage has led states to buy these masks from uncertified foreign producers or from producers that sell foreign-certified products.
“Every state has had to go and buy whatever they can find,” says William Herzog, an assistant leader of the Advanced Materials and Microsystems Group at MIT Lincoln Laboratory. “There’s potential for fraud when buying masks not certified by a U.S. agency. So, there’s a need for assessing the performance of these foreign or uncertified masks — people want to know if they’re effective.”
Lincoln Laboratory is part of a coalition working with the Massachusetts Manufacturing Emergency Response Team (M-ERT) to test the quality of N95s, KN95s (N95-like respirators that are made and certified in China), and materials that companies wish to use to make N95 masks.
Since the effort began about two weeks ago, the Laboratory has tested several dozen different mask products in two ways. The first test measures filtration efficiency, determining what percentage of particles of a certain size the mask keeps out. The other test looks at liquid penetration. For this test, the researchers simulate blood spatter and assess whether it can soak through the mask.
The Laboratory is not certifying respirator masks with its testing; only the U.S. National Institute for Occupational Safety and Health (NIOSH), or NIOSH-certified laboratories, can do that. However, the tests are conducted following NIOSH testing protocols and instrumentation as closely as possible. The aim of the tests is to help public officials and healthcare providers gauge the effectiveness of this personal protective equipment (PPE); the test results are being published on the Massachusetts Department of Public Health’s website for PPE guidance.
“People are looking for answers,” Herzog said. “We had a fire marshal walk into our lobby with masks for us to test. So, the goal is to have a place where hospital administrators, fire and police departments, health care workers, or really anyone can look up whether the mask they bought is effective or not.”
Through M-ERT, the Laboratory is working with the Advanced Functional Fabrics of America (AFFOA), a manufacturing innovation institute in Cambridge, MA, to obtain masks for testing. Michael Rein, senior product engineer at AFFOA, says that besides receiving masks from the state to test, AFFOA is receiving testing requests from hospitals, small businesses, academic groups, and large commercial companies. “We receive the materials and masks, prioritize them for testing, and then connect them to a partner lab for testing,” Rein says.
Lincoln Laboratory is one of these partners, in addition to the University of Massachusetts Lowell, the U.S. Army Combat Capabilities Development Command Soldier Center, and MIT Professor Gregory Rutledge’s laboratory on campus. Prof. Rutledge’s early efforts to test the filtration efficiency of masks have complemented the Laboratory’s own filtration work.
According to the NIOSH specification, N95 (and Chinese-certified KN95) masks should filter out at least 95% of particles of a certain size. The test equipment that NIOSH uses to certify masks, however, is “highly specialized and hard to come by” says Shane Tysk, who has been leading the filtration efficiency testing at the Laboratory. Thus, the Laboratory has had to build its own setup with the goal of obtaining similar results.
To test for filtration efficiency, the setup generates aerosols of salt particles at a certain size. Then, the aerosol-laden air is drawn down through a test fixture that holds a sample of the mask materials and into a collection chamber, where the researchers can measure the particles that made it past the mask filter. At the same time, they measure the pressure drop across the mask, which indicates inhalation resistance, or how hard it would be for someone to breathe with the mask on. To date, they’ve tested multiple copies of more than 70 different kinds of masks.
Tysk says that when comparing the performance of the KN95 masks in their test to that of certified N95 respirators, only about half are passing the 95% filtration efficiency standard. The tests at the Laboratory are focused only on particles ranging in size from 300 nanometers to 10 micrometers. Picture the size of a droplet expelled by coughing, sneezing or talking, and which might house a clump of viral particles. Prof. Rutledge’s testing on campus is measuring particles smaller than 300 nanometers, at the scale of a single coronavirus particle. The two teams’ filtration efficiency results have differed in some cases.
“Results can be both correct and not exactly the same depending on how the measurement was conducted. Filtration efficiency curves vary with particle size,” Tysk says. “It’s difficult when the question is simple, for example ‘is this mask good?’ but the answer might be complex. In this situation, our testing and MIT’s are complementary — if you put our particle range results together, you get a very detailed measurement.”
In addition to testing filtration efficiency, the Laboratory is also testing N95 and KN95 masks’ resistance to blood penetration. While not all N95 masks are designed or certified as a surgical mask, surgical-grade N95s, and their KN95 counterparts, must protect people both from the inhalation of aerosols and from splashes or sprays of body fluids.
Andrew Whitehead in the Rapid Prototyping Group built the Laboratory’s own blood-spray setup following ASTM International synthetic blood test standards. Prior to testing, masks are preconditioned in a humidity chamber to simulate exposure to moisture from the wearer’s breath, which can impact permeability (preconditioning is also done for masks undergoing aerosol testing).
Each mask is sprayed from a distance of one foot with two milliliters of synthetic blood at one of three velocities, simulating what a surgeon would experience when puncturing a blood vessel at various blood pressures (80, 120, or 160 mmHg). Then, the researchers visually inspect the inward-facing side of mask and use a swab to check if any liquid has soaked through.
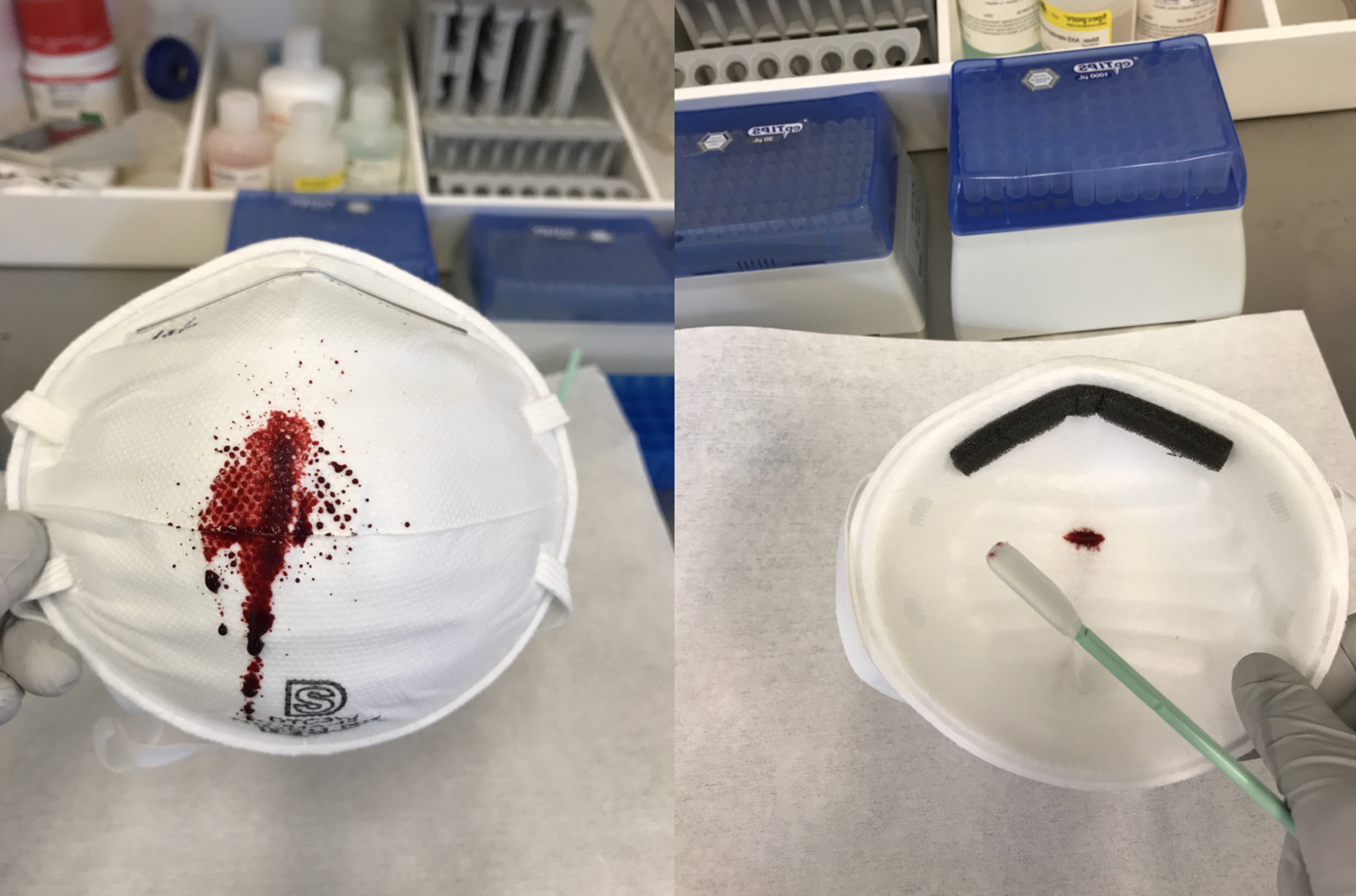
“Unlike a lot of the testing we do here, this is very much a qualitative test. We’re visually checking to see if the other side of the mask is wet. A clean surface passes,” says Lalitha Parameswaran, who has been leading this testing. So far, her team has tested 58 different kinds of masks, with six replicates of each. About 70 to 80 percent of the masks have passed, though Parameswaran says that they are refining the test to add inspections after a period of time to check for seepage.
Of course, to be effective the masks also need to fit properly, forming a tight seal against the face. The Laboratory is not testing the masks for fit. But with these filtration efficiency and liquid penetration data, the researchers are helping manufacturers know quickly whether or not the materials they plan to make surgical masks and N95 masks with will work, and if foreign-acquired masks are of good quality.
The Laboratory plans to double their testing capacity soon, thanks to more funding they’ve acquired. All of the testing done through the Laboratory, and through AFFOA, is currently provided as a free service to those who request it.
“It’s very important for people to understand how well their PPE works,” Tysk says. “It’s a fulfilling thing to do. It’s been a real time crunch to do it quickly and to do it right, but it’s something that really matters.”
Rein adds that he is “very grateful to have test partners in MIT and Lincoln Laboratory to help in this effort. Donating their time is not trivial, and they’ve gone so above and beyond to be able to set this up.”
The researchers wish to thank all staff who have been critical in standing up the testing at the Laboratory. This team includes Alberto Cabral, Joseph Chludzinski, Jude Kelley, Paul Robinson, Devon Beck, and the Engineering Division at Lincoln Laboratory.
