Steady demand for PPE may encourage local businesses to start up production

Without a vaccine for COVID-19, health care and other frontline workers must rely on personal protective equipment (PPE) to guard themselves from exposure to the novel coronavirus. Demand for PPE has been substantial in Massachusetts since the outbreak began. What's unclear is just how great the demand will remain going forward, and if the state is equipped to meet it.
To help settle this uncertainty, Lincoln Laboratory conducted a study to estimate demand for PPE in Massachusetts over the next 18 months, specifically for N95 and surgical masks, gloves, and surgical gowns. The analysis was conducted for the Massachusetts Manufacturing Emergency Response Team (M-ERT), a coalition stood up by the governor in April to help manufacturers produce materials needed in response to the pandemic.
The goal of the study was to inform local companies of the PPE demand, so that these companies can best decide whether or not to shift their operations to manufacture PPE. The team recently presented its findings to M-ERT along with industry leaders in the state.
"While it seems obvious that demand for PPE is high, some Massachusetts manufacturers have been searching for strong data to confidently turn over their operations and pivot to producing PPE," says Carolyn Kirk, the executive director of the Massachusetts Technology Collaborative, which leads the work of M-ERT. "The work of MIT Lincoln Laboratory's PPE demand modeling team has provided a thorough analysis of projected demand over the medium term that tracks alongside anticipated and continued impacts of COVID-19."
Outbreak modeling
The Laboratory's approach to estimating PPE demand considers two needs: the in-hospital demand that scales with the number of hospitalized COVID-19 patients, and the in- and out-of-hospital demand that must be sustained over the outbreak duration for frontline workers.
To predict in-hospital PPE demand, the team first developed an outbreak model to estimate COVID-19 hospitalizations under different intervention strategies. This modeling work was done in mid-April. For a stay-at-home scenario, like that implemented in Massachusetts until the phased reopening began on May 18, the model showed the outbreak peaking on April 21, 2020, with more than 4,000 hospitalizations and tapering off around April 2021 with hospitalizations near zero.
They then modeled hospitalizations in an example "intermittent-intervention" scenario, which may better represent reality moving forward. This scenario consists of cycles of "open" society with people going out, causing the virus to reproduce and increase hospitalizations, followed by "closed" periods with protective measures to gain control over the outbreak. These cycles carry on over time, with hospitalizations gradually decreasing and the outbreak extending through November 2021, at which time we may optimistically have a vaccine.
"We have this data-driven model that feeds our estimates. Whichever COVID-19 intervention strategy is implemented, whether it's lockdown or reopening or something in between, we can turn the knobs on the model to predict the hospitalizations and the duration of the outbreak, which impact our PPE demand projections," says Lisa Wei, who conducted the study with fellow Laboratory staffers Cassandra Smith, Megan Richardson, and Kevin Tangen.
PPE projections
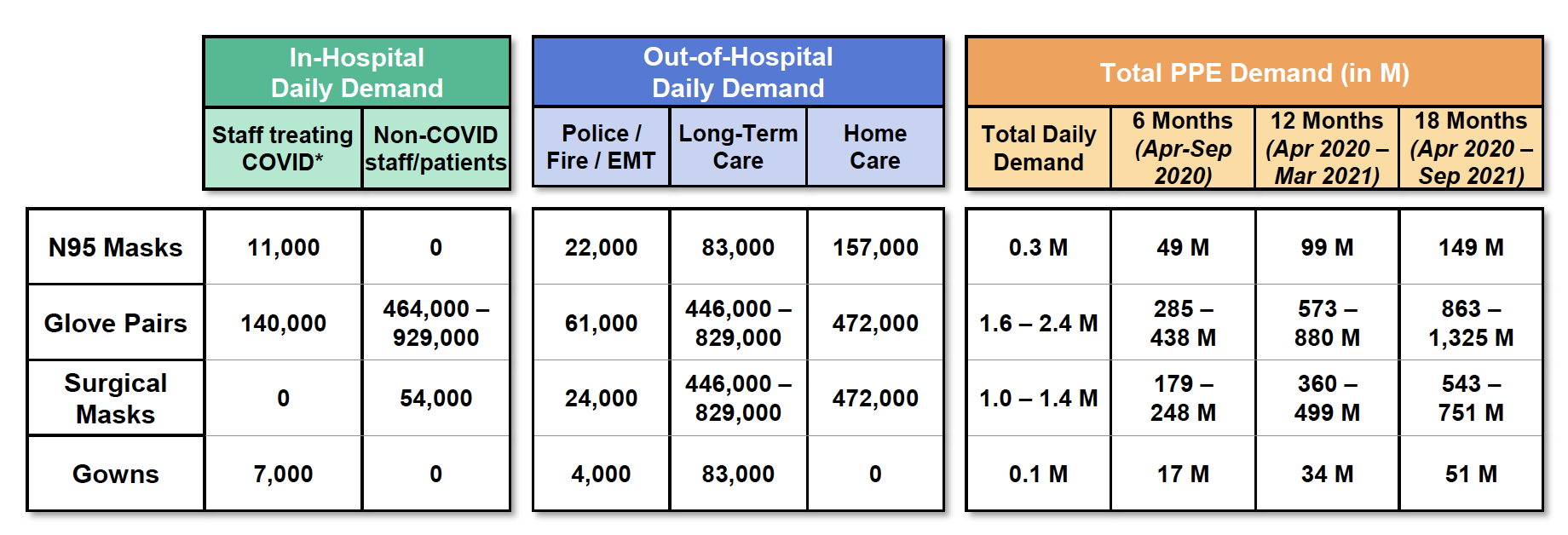
Under the intermittent-intervention strategy, the team estimated daily in-hospital demand to be about 11,000 N95 masks, 54,000 surgical masks, 600,000 glove pairs, and 7,000 gowns. Daily out-of-hospital demand for N95 and surgical masks is about 25 times that of in-hospital demand, and about 12 times the in-hospital demand for gowns. Gloves are comparable.
Taken together, the daily PPE demand averaged over 18 months is approximately 300,000 N95 masks, 2 million glove pairs, 1 million surgical masks, and 100,000 surgical gowns.
"We had initially thought that demand would be driven primarily by the protection of hospital staff. It was eye opening to see the amount of potential demand for PPE needed outside of the hospital to protect first responders and long-term and home care staff," says Diane Jamrog, who advised the team with Pamela Evans.
For in-hospital demand, the team consulted local medical experts, COVID-19 hospitalization and PPE usage data from Beth Israel Deaconess Medical Center, and staffing data from the American Hospital Association in Massachusetts to estimate how much of each type of PPE is consumed per day. They also modeled the likely distribution of patients in the hospital and their disease progression. Those details impact staffing levels and PPE usage. For instance, doctors and nurses treating COVID patients in the ICU each use on average four N95 masks and surgical gowns per shift, versus two of each per shift when treating patients on the hospital floor, according to published pandemic recommendations. The estimates also capture the steady PPE use by staff treating non-COVID-19 patients, and PPE that are given to each patient as they enter a hospital.
Out-of-hospital demand covers the PPE needs per shift of police, firefighters, and EMTs; long-term care facility staff; and home health aides. The researchers looked to first responder staffing data from the U.S. Bureau of Labor Statistics and long-term and home care staffing data from the Massachusetts Healthcare Chartbook, and interviewed leaders of care organizations and fire departments to understand usage rates. They learned, for example, that firefighters and EMTs are expected to change their N95 mask and gloves with each call, and that a station may receive anywhere from five to 20 calls per shift.
"Going in we just didn't know how much PPE people were using — there were reports on availability, best practices, and some literature," Richardson says. "We were able to take a major step when we could reach organizations about their numbers of PPE per shift and how they're using it. We tried to pull in as many others as possible."
The researchers also estimated PPE demand under the sustained stay-at-home scenario. When comparing those totals with the intermittent-intervention totals over the next three, six, and twelve months (at which time the outbreak would end under the stay-at-home scenario), PPE estimates differed by just five percent. However, extending the outbreak an additional six months under the intermittent-intervention scenario increases cumulative demand by 50 percent. That translates to an additional 52 million N95 masks.
"We expect PPE demand to peak and wane given intervention strategies and people's behavior around those," Wei says. "Part of the motivation of this study was to capture that uncertainty of the future."
Decisions ahead
As the outbreak goes on, the researchers note that their methodology can be used to incorporate updated data and include a wider range of PPE consumers that this study didn't consider, such as dentists and physicians. Demand for PPE could also grow as schools and more businesses in New England reopen.
"The value of this study is really in giving perspective," Evans adds. "If there are companies that want to transition to producing PPE, companies that have had to shut down, we're producing data to show that it may be a wise business decision."
Businesses in Massachusetts have already begun shifting their operations to meet PPE needs. New Balance, as one example, opened its shuttered factories in early May to produce face masks, and more than 450 other local companies have expressed an interest in working with M-ERT to produce various PPE, says Kirk. But motivating more businesses to transform their factory floors to meet supply deficits is difficult without data to look to. This study has helped fill that analysis gap.
"Like good public health data, good business data is also important for decision making," Kirk says. "Lincoln Laboratory has performed a vital public service with its demand study, and its lasting contribution will be seen in the growth of domestic manufacturing and jobs here in Massachusetts."